Croup in Children: Symptoms and Treatment. Dr. Narmin Azizova
Croup in Children: Symptoms and Treatment
Dr. Narmin Azizova
General Information
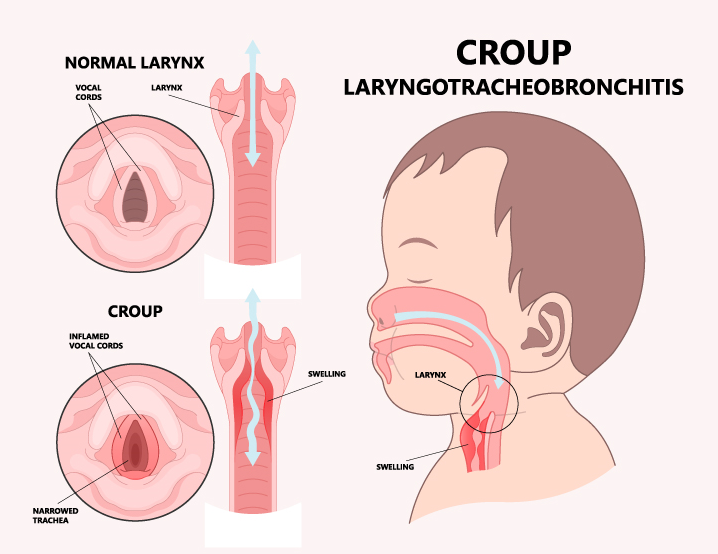
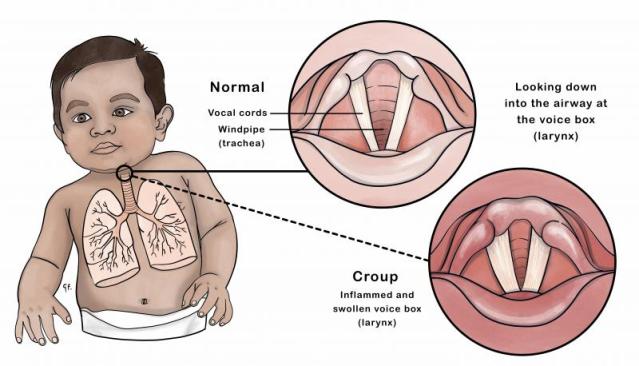
Croup is an infectious disease characterized by inflammation and swelling of the upper respiratory tract, particularly the larynx (vocal cords) and trachea. It is most commonly observed in children between the ages of 6 months and 3 years. In children older than 6 years, croup is rare. This condition is more frequently seen at the beginning of the fall and winter seasons.
Even a small amount of swelling in the airways can lead to significant narrowing and an increased rate of breathing. Viruses are the main cause of croup, with the most common being parainfluenza virus, respiratory syncytial virus (RSV), and influenza viruses.
Croup can spread from an infected child to a healthy one, primarily through droplets released when coughing or sneezing. The infection can also be transmitted via objects used by the infected child. If a healthy child contracts the infection, symptoms may develop within 2-3 days.
Symptoms of Croup in Children
Croup typically begins with mild fever, runny nose, pharyngitis (sore throat), and a mild cough that lasts a few days. Suddenly, especially at night, children may develop a distinct “barking” cough, hoarseness, and stridor (wheezing sound during breathing), accompanied by chest retractions (when the chest muscles are visibly pulling in with each breath). The typical complaint that drives parents to seek emergency care is the loud, barking cough and associated stridor that awakens the child during the night. As the obstruction of the upper airway worsens, the child may experience difficulty breathing, fast breathing, restlessness, and a bluish tint around the mouth, nails, and lips (cyanosis). During this time, the child may have a mild fever, but in some cases, the temperature can rise as high as 39-40°C (102-104°F). Some children may not exhibit a fever.
When a child experiences a barking cough, they may adopt a forced position, such as sitting up or standing, to ease their breathing. This condition typically improves over several days and most cases resolve within a week.
For older children, symptoms may be milder. During episodes of difficulty breathing, children and their families may experience fear and anxiety, which can worsen the situation. Anxiety in children can lead to increased crying, which in turn can intensify the symptoms. In severe cases, children may not have a barking cough, but chest retractions can still be observed.
When to Seek Hospitalization
Immediate medical attention should be sought if any of the following occur:
- Difficulty breathing
- High fever
- Barking cough
- Hoarseness or a rough voice
- Cyanosis (bluish color around the skin and nails)
- Chest retractions (visible pulling of the chest during breathing)
What to Do Initially if Croup is Observed?
Croup can be frightening for both children and parents, as respiratory distress can escalate quickly.
To relieve symptoms, having the child breathe cool air for 10-15 minutes can help reduce the swelling in the airways. Taking the child outside to breathe cool air or using a humidifier near the child can also help ease the symptoms. Moist air reduces the swelling of the vocal cords, helping to improve breathing. For infants and young children, nasal congestion can further complicate breathing, so saline nasal sprays or drops can be used to clear the nasal passages.
Raising the child’s head while they sleep can also facilitate easier breathing. If the child has a fever, antipyretics can be administered to lower the temperature.
It is essential to contact a doctor when croup is suspected. In more severe cases, hospitalization may be necessary. The treatment administered by the healthcare provider (oxygen, steroids, and inhaled adrenaline) can help the child recover more quickly.
Additional Notes:
- Croup’s Characteristic “Barking” Cough: One of the hallmark symptoms of croup is a harsh, “barking” cough that sounds like a seal or dog. This is due to the swelling and inflammation of the airways, particularly the larynx, which narrows the airway.
- Age Group Most Affected: Croup is most commonly seen in children between 6 months and 3 years of age because their airways are smaller and more susceptible to swelling.
- Symptoms Worsen at Night: Croup symptoms, particularly coughing and difficulty breathing, tend to worsen at night. This is because the child’s airways tend to swell more while they are lying down.
- Difficulty Breathing: In severe cases, croup can lead to significant breathing difficulty, including stridor (a high-pitched wheezing sound), rapid breathing, and chest retractions. If left untreated, these symptoms can become more severe.
Treatment and Medical Intervention
While most cases of croup can be managed at home with supportive care, more severe cases require medical intervention. In some instances, medications such as corticosteroids or nebulized adrenaline may be used to reduce inflammation and open the airways. In rare cases, the child may need to be hospitalized for more intensive treatment, including oxygen therapy.
Statistics and Global Health Considerations
According to the World Health Organization (WHO), respiratory infections, including viral croup, are among the leading causes of hospitalization in young children worldwide. In the United States alone, approximately 3 million cases of croup are reported annually, with the highest incidence occurring between the ages of 6 months and 3 years. WHO also highlights that viral croup has a seasonal peak, typically in the fall and winter months, coinciding with the highest circulation of respiratory viruses.
Summary
In conclusion, croup is a common viral infection in children that leads to inflammation and narrowing of the airways, resulting in a barking cough and difficulty breathing. While most cases can be managed at home, more severe cases require medical attention. Parents should monitor their child’s symptoms closely and seek medical help if breathing becomes difficult or the child shows signs of significant distress.